What is Quality and Patient Safety?
Quality has been defined by the federal Agency for Healthcare Research and Quality (AHRQ) as “doing the right thing at the right time for the right person and having the best possible result.” Patient safety is simply defined by the World Health Organization as “the prevention of errors and adverse effects to patients associated with health care”.
Cooper University Health Care takes a comprehensive approach to evaluate the quality and safety of each patient’s experience. Our patient care delivery model is continuously reviewed, analyzed, and improved and consists of:
- Identification and adherence to evidence-based practices and comparative measures evaluating management of outcomes and chronic conditions to ensure better patient outcomes and lower costs of care.
- Timely and effective access to care.
- Observance of 18 hospital patient safety indicators for patient care.
- Focus on clinical outcomes in comparison to other leading health care organizations and national benchmarks of care.
- Coordination and management of chronic conditions and care transitions.
How is Quality and Patient Safety measured?
 Cooper University Hospital evaluates the quality of care by measuring whether it is effective, timely, safe, and responds to our patients’ preferences and needs. Our Quality Improvement Model is based on the expectation of continuous improvement where performance is evaluated in an atmosphere that supports openness and transparency.
Cooper University Hospital evaluates the quality of care by measuring whether it is effective, timely, safe, and responds to our patients’ preferences and needs. Our Quality Improvement Model is based on the expectation of continuous improvement where performance is evaluated in an atmosphere that supports openness and transparency.
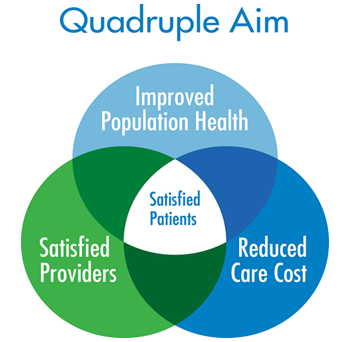
Following the "Quadruple Aim" approach developed by the Institute for Healthcare Improvement (IHI), Cooper uses multiple approaches to measure the delivery of quality patient care.
Enhancing the Patient Experience
- Improving communication with doctors, nurses and responsiveness of hospital staff.
- Improving responsiveness to pain management.
- Providing a clean and safe hospital environment.
- Providing clear and understandable discharge information.
- Reviewing patients self-reported experience results from the Hospital Consumer Assessment of Healthcare Providers and Systems Hospital Surveys (HCAHPS) to convey aspects of care that we have opportunity to improve our delivery of care.
Improving Population Health
- Implementing evidence-based practice and core measure compliance.
- Reducing in hospital readmissions, mortality rates, and hospital acquired conditions.
- Reducing in errors related to complications.
- Evaluating outcomes that measure the cost of care delivery and level of care provided for the below matrix:
- Inpatient stroke
- Venous thrombolytic embolism (blood clots)
- Sepsis
- Immunizations
- Perinatal care
- Emergency department throughput
- Outpatient emergency department pain management
- Outpatient colonoscopy follow up
Reducing Costs
- Reducing in readmission expense.
- Reducing in spending for workers’ compensation claims.
- Reducing employee injuries.
- Reducing medical error litigation.
- Improving employee productivity.
Improving Professionals Work Life
- Preventing and identifying health care professional burnout.
- Documenting into electronic health record by dedicated teams, which has been associated with increased staff satisfaction, improved revenues and the capacity of the team to manage a larger volume of patients (i.e. clinical documentation specialists). (Bodenheimer T, 2014)(Reuben DB, 2014)
- Standardizing workflows which result in improving employee satisfaction.
